Healthcare KPIs and Metrics to Measure (with Examples)

Cultivating a workforce culture that embraces continuous improvement and establishing a process to review and act on the results, are the foundations to establishing key performance indicators (KPIs) and other metrics to measure in your healthcare business.
In this blog, we look at two ways healthcare providers can measure their performance:
- Patient satisfaction
- Healthcare organisation performance
Know the why
Keep your colleagues and staff informed of why you’ll be measuring healthcare KPIs. This could be to improve areas of weakness and to celebrate your businesses’ successes.
Let staff know how they and their patients will be informed of findings and get them onboard with the measurement process.
Identify a champion, such as a practice manager who will be responsible for implementing the activities and driving the action plan.
What are the top issues
Most business owners have an idea of what the top issues are that need to be addressed.
Among others, issues could include:
- reviewing staff to patient ratio
- reducing patient wait time
- improving overall patient satisfaction
- reducing healthcare costs
- reducing missed appointments
- generating new patients
- using staff resources more effectively
- increasing profitability
- reviewing average length of visit.

Patient satisfaction surveys
Patient satisfaction surveys can help identify ways to improve your healthcare service, ultimately translating into happier patients and more return customers.
Patient satisfaction surveys also demonstrate to your patients that you care and you’re interested as a healthcare provider in providing high quality patient care and positive outcomes.
When designing a survey:
- Keep it brief and simple. The longer the survey the less likely it is to be completed.
- Use consistent scales e.g. 10 point scale or five point scale for all scale questions.
- Include at least one open ended question e.g. ‘Is there anything else you’d like to tell us to improve your experience?’
- Collect demographic data. This data can tell you whether you’re hearing from a representative sample of your patient group or help you improve in areas targeting specific demographics e.g. accessibility for older people.
- Aim for anonymity with the option for a person to provide their contact details if they wish to receive follow-up. This will improve the response rate of your survey.
Choose the right tool
There is a huge range of tools available such as SurveyMonkey, SnapForms, HappyorNot and RapidReviews among others.
Choosing the best tool for your healthcare business could be determined by cost and length of your survey.
Other considerations include:
- The issues you’re aware of that you’re trying to solve.
- The length of the survey. Are you looking for a quick ‘net promoter’ score about the patient’s experience as they pay to leave? Or do you want something more detailed that provides insights into the patient experience from booking, clinician care and follow-up to patient outcomes?
- Consider the accessibility of patients who are vision impaired, need information in alternative languages and the access they have to technology such as smart devices.
- Consider infection and prevention control. A survey on a patient’s own device is more hygienic than a pen and paper version. But if you need to use a public device such as a touchscreen to improve response rates, provide hand sanitiser alongside it.
Focus groups
A focus group is a facilitated discussion among a selected group of patients. This method enables healthcare organisations to collect qualitative feedback from patients and tease out information on subjects in greater detail than a survey allows.
A focus group may be suitable if you’re wanting to find out about the patient satisfaction of a specific group, for example patients with disability and their carers.
It could also be used to collect feedback from patients unlikely to respond to a survey. For example you could have translators with a focus group of non-English speaking patients.
An experienced and trained professional moderator is key to a successful focus group. Their role is to keep the conversation on track to ensure the discussion provides meaningful information that the healthcare organisation can act on, encourage discussion, ensure everyone has the opportunity to have their say and manage the conversation in a safe way.
Focus groups are time intensive to organise and synthesise the findings and can be more costly than other methods of measuring patient satisfaction, but can be worth the investment.
Patient interviews
A structured discussion between a patient and interviewer over a series of planned questions is another way to gain patient feedback that may be more open than feedback provided in a group setting.
Interviews are also preferred if discussing a sensitive topic, particular instance of the patient’s experience or experience with an individual healthcare provider.
You may even handpick patients who are representative of a wider patient group such as patients with a particular chronic disease.
Align to your business goals
Healthcare businesses often have similar goals around providing high quality and safe healthcare that improves patient outcomes. Remember to ask the key questions which align with your business goals, such as ‘overall how satisfied are you with the quality, safety and outcomes of your healthcare’?
Learning from your patients
The Royal Australian College of General Practitioners has developed a Patient feedback guide: Learning from our patients to assist general practices to:
- understand what is required to fulfil Criterion 2.1.2 of the RACGP Standards for general practices (4th edition)
- explain the options available to practices for meeting the requirements of criterion 2.1.2
- provide guidance for practices wishing to develop their own practice-specific patient feedback tool.
The RACGP Toolkit for developing practice-specific questionnaires is a separate document to be used in conjunction with the Guide. It provides resources to assist practices in designing a practice specific questionnaire and is available for free download.

Healthcare organisation performance
Data has the power to transform your healthcare practice if used well. You probably already have access to metrics in your healthcare facility, it’s just a matter of using these metrics to improve operational efficiency and patient satisfaction.
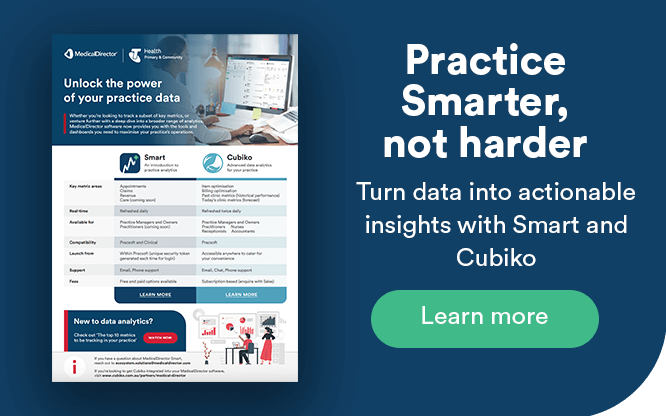
Introducing Smart
Smart is a new feature soon to be available in MedicalDirector’s Pracsoft and Clinical solutions that provides a visual dashboard of key metrics such as:
- average patient wait time
- open appointments
- non-attendance
- immunisation eligibility
- GP consulting metrics including appointments per day and prescribing trends enabling comparison between clinicians within a practice
- consult volumes, billings and trends over time to accurately forecast revenue and reduce administrative overheads.
Smart gives you access to your practice data in easy to understand visuals – helping you reduce practice wait times, improve the patient experience and better support your practitioners.
Smart is easy to integrate with your practice management and clinical software, keeping your data safe.
It can be used by anyone from across the business including practice managers, clinicians and business owners.
To access Smart in your existing Clinical or PracSoft solutions, or if you’re a new customer, click here.
In the coming months, MedicalDirector customers will have the opportunity to integrate their practice and clinical management software with Cubiko for more detailed actionable insights.
Cubiko can also enable comparison across different practices and different databases.
Acting on the findings
Review feedback and determine which issues will be acted on as a priority. Ensure any feedback received that requires a prompt response is acted on quickly.
Embedding changes into your healthcare organisation requires an action plan such as a Plan, Do, Study, Act (PDSA) Cycle. PDSA Cycle is commonly used in healthcare organisations worldwide to drive continuous improvement in healthcare KPIs.
The PDSA cycle is shorthand for testing a change by developing a plan to test the change (Plan), carrying out the test (Do), observing and learning from the consequences (Study), and determining what modifications should be made to the test (Act).
Close the loop with your patients. Let your patients know how their feedback has influenced improvements e.g. reductions in patient wait times, improvements in patient safety, staff to patient ratios, patient follow up rate or the patient experience.
Finally, healthcare KPIs should be embedded in your organisation. Ensure there are ongoing methods for patients to provide feedback e.g. via an email listed on your website for complaints, compliments and other feedback or a SMS survey following each appointment.
Your interest in patient satisfaction is also a great marketing tool for your business and shows you care about healthcare quality.
Resources
- Plan, Do, Study, Act (PDSA) Cycle Worksheet
- RACGP’s Patient feedback guide: Learning from our patients
- RACGP’s Toolkit for developing practice-specific questionnaires
- MedicalDirector Smart
- Cubiko