Eclipse Claims are direct communication for providers with Medicare and the Health Fund in one transaction. Eclipse Claims (no gap) amounts are as contracted with the Health Fund and the Practitioner. This handout will assist with explaining the process and the resulting report for tracking your claim
Eclipse Claims with no gap require a single account; the Eclipse account for claiming with Medicare. The following steps are required for completing a claim:
1. Search for the required patient
2. Search for existing Eclipse account, or create a new account
3. Issue the invoice
4. Send off Eclipse claim to Medicare
5. Access the Eclipse report; Inpatient Medical Claim Report
Procedure
1. From the Patient Details screen, select the Accounts menu item, and locate an existing Eclipse account.
o If an Eclipse account exists, right-click it and select Open Account. Proceed now to step 6, to issue the invoice to bill the Patient.
o If an Eclipse account does not exist, create a new Eclipse account. Continue now to Step 2.
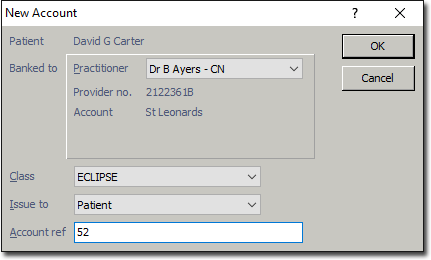
2. Click the New button. The New Account window appears. Select the required Practitioner, Class as Eclipse and click OK.
3. The Account Details window appears.
o Select Health Fund Membership as New.
o For the Health Fund field, either enter or click into the list to select the required fund.
o Enter the Account Name as on the health card. If the name differs, select the option above Health Fund.
o Enter the Membership No. , Ref No. and select the Default Membership option. This will generate the details onto the Patient Details screen.
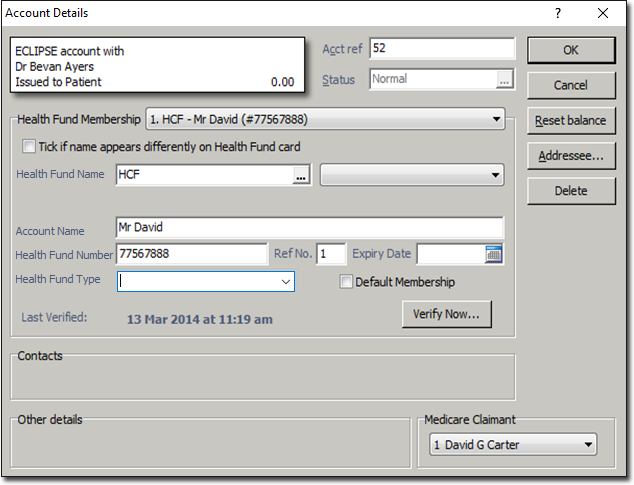
Note: If a Health Fund has been previously entered, it will automatically appear in the Health Fund drop down list.
4. Click Verify Now to verity the Health Fund, clicking OK through the prompts, and then click OK to save the account.
5. Open the Eclipse Account; right click and select Open Account.
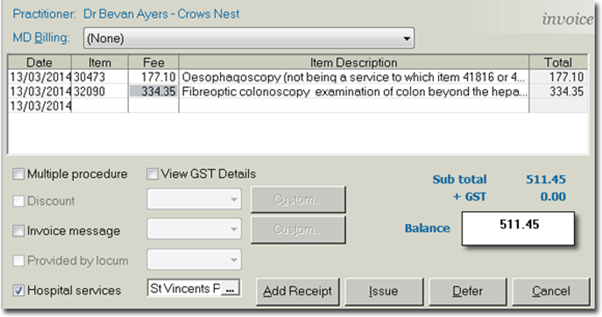
6. Issue an invoice for the Eclipse claim.
o Click the New Invoice button
o Click OK or Continue to the verification prompt
o Enter Item numbers required to populate total amounts
o Tick Hospital Services and select Hospital
o Click Issue, select Referral, and OK for date
7. Click the IMC Submission button to display the New Inpatient Medical Claiming window.
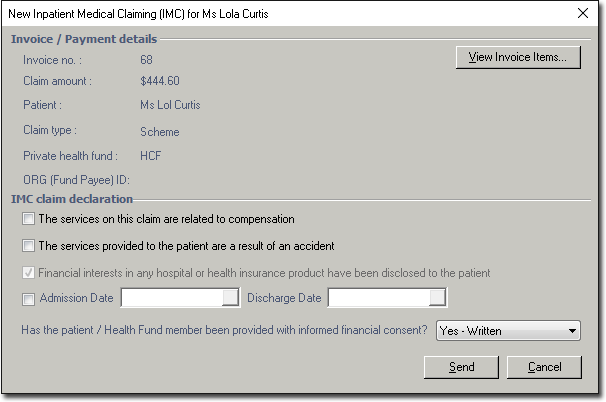
8. Always; select Yes – Written when prompted ‘Has the patient/Health Fund member been provided with informed financial content’, and then click Send to transmit the claim to Medicare.
Note: If a Practice is setup as Agreement, there will be two options for Has the patient/Health Fund member been provided with informed financial consent. Yes – Written or Yes Verbal.
9. Open the Private Account, by selecting Accounts from the margin menu; double clicking on Private account or, highlight and click on the Open Existing Account button.
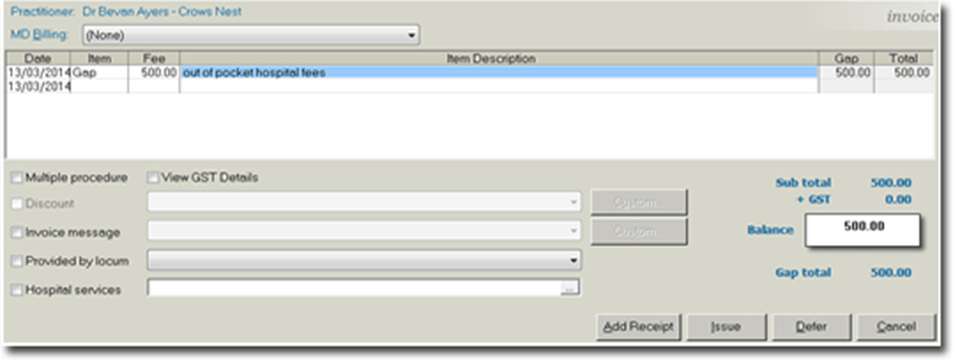
10. Issue an invoice for the Patients gap.
o Click New Invoice.
o Enter Item number which will auto-populate an amount (if setup) or manually enter the amount.
o Click Add Receipt.
o Select Referral, and click OK to the date.
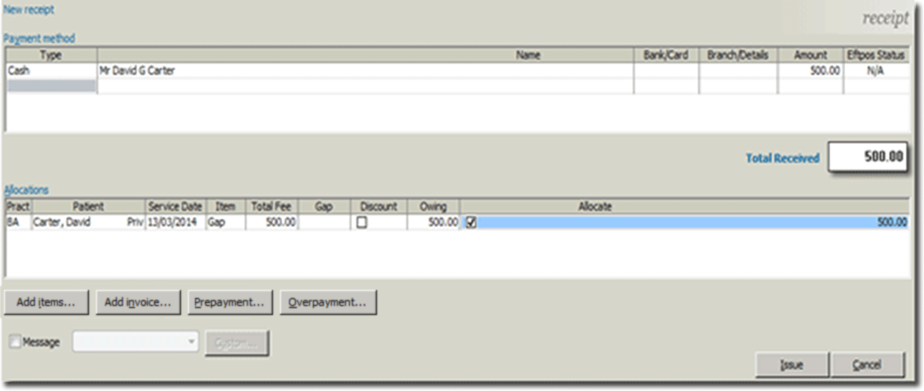
11. The New Receipt window appears. Select a payment Type from the drop down menu, enter the amount, and allocate the invoice amount to the receipt amount by clicking the open box (right of amount). This will display a tick, click Issue, click OK to date; select receipt and File or Print.
Eclipse (IMC) Claim – Medicare Australia Module
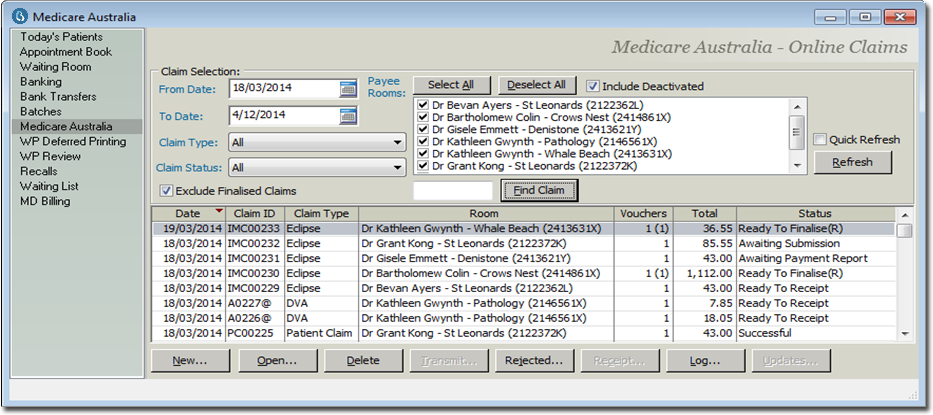
When Eclipse claims are submitted within a Patients account, the claim generates into the Medicare Australia module. To access; click into Practice Explorer, and from the margin menu click on Medicare Australia. These claims are waiting to be processed, ready for action or rejected and waiting to troubleshoot depending on the Status.
You can view claims associated with individual or all Practitioners. You can examine claims within a specific date range, individual or all claim types and indicate to display finalised claims. When changes are made to these options, ensure you click on the Refresh button or the Quick Refresh check box is selected to auto-refresh display. The status of claims determines the action required on the claim.
The following statuses will display once an IMC Submission has been submitted to Medicare.
|
Claim Status |
Description & Action |
|
Awaiting Submission |
Claim is waiting to be sent to Medicare. Click on the Transmit button. |
|
Awaiting Processing Report |
Waiting for the processing report for the claim. It can take up to 3 business days to process. Click on the Transmit button to retrieve the process report. |
|
Awaiting Authorisation |
Claim requires to be authorized. Open the claim and send to Medicare from the edit screen. |
|
Awaiting Payment Report |
Claim has been successfully processed, however awaiting payment report. It can take up to 6 business days to process. Click on the Transmit button to retrieve the payment report |
|
Ready to Receipt |
Claim has been successful in processing and payment with Medicare. It is ready to receipt. Reconciling with the Bank Statement and payment is recognized, click on the Receipt button. Once receipted; the receipt will generate to the Banking, EFTPOS, as a Direct Debit payment. |
|
Rejected |
Items within the claim have been rejected. Click on the Reject button to display the Medicare Error Code & Description, and to decide to resubmit or write off the claim |
Eclipse Reports
Bluechip provides many Medicare Reports that can assist with claiming and reconciling. Three reports as a quick reference to assist with Eclipse Claims are:
o Debtor Detail Report: provides a summary and detailed breakdown of patient account balances by duration of time (ageing). This will generate the outstanding debit for Eclipse claim accounts.
o Inpatient Medical Claim Processing Report: provides a list of unprocessed and processed Eclipse claims. In the Medicare module; these are the Eclipse claims status Waiting Process Report, Waiting Payment Report, Ready to Receipt, Rejected and Finalised (Receipted), etc.
o Inpatient Medical Claim Payment Report: provides a summary and detailed list of processed Eclipse claims that generate the Medicare and Health Fund payment for the claims. This report can be used to reconcile the Practitioners bank statement. . In the Medicare module paid Eclipse claims generate the status Finalised (Receipted).