Reducing the cost of chronic disease
Reducing the cost of chronic disease
Chronic diseases account for 90% of all the deaths in Australia and the total annual cost of Australian hospital stays is a staggering $15.1bn.* So what can we do to reduce the increased burdens faced by hospitals while improving patient outcomes?
According to the Australian Institute of Health and Welfare (AIHW), on an average, 23,000 people are admitted to hospital every day in Australia. Among the chronic conditions, the 2 major ones are diabetes and cardiac conditions that lead to more than 70% of mortalities. In fact, diabetes & hypertension have become a major epidemic worldwide and represent a significant burden of morbidity and mortality to the aging Australian population and to healthcare budgets. This burden is increased by the secondary medical conditions that may arise as a consequence of these conditions.
But according to RACGP*, over 30% of all hospitalisations can be avoided by better management of chronic conditions. In fact, enabling the patient to take control of their health and also providing a cost-effective solution to both the patients and healthcare provider has been the main focus for the Australian Government and also the newly launched program – Health Care home.
On top of this, clinic visits can represent an important cost for both the health-care system and for patients. There is a growing recognition of the need to reduce clinic costs by avoiding unnecessary visits or Potentially Avoidable Hospitalisations (PAH). At the same time, improved data capture and transmission to clinicians in real-time would allow timely review of critical clinical data, early response to poor management and adjustment of clinic visits to optimise care for those requiring support and to respect and reinforce the positive status of those effectively managing their condition.
A more effective method of communication to help manage chronic disease
Telehealth technologies have been shown to have the potential to provide more effective medical communication between patients and healthcare professionals in a range of chronic conditions** including diabetes, cardiac conditions and chronic respiratory disease. When we say Tele-Health, the first picture that comes to anybody’s mind is a patient sitting in front of the computer monitor talking to their doctor. However, video consultation is only a component of the entire Tele-Health spectrum. In fact, Telehealth can be categorised into 3 components: channel (video consultation), decision support tool (remote monitoring) and active coaching and motivation tool (tele coaching).
These 3 components form the entirety of telehealth that enables patients to take control of their health with the support and motivation from health providers with improving the quality of patient- centric care.
A decision support tool that’s proactive about chronic disease
One of the ways telehealth technologies can offer a more proactive approach to managing chronic disease is the decision support feature. Real-time transmission of key health indicators, such as blood sugar measurements in diabetes along with meal and medication details, allows healthcare staff to assess patients quickly and regularly, rather than through a review at standard clinic visits. This allows the identification of changes or trends that may require intervention, and provides clinicians with the opportunity for prospective and proactive health care.
Similarly, appropriate levels of reduced care can be offered to well-controlled patients saving the patient and healthcare system time and money.**
Already, the use of remote medical care and monitoring through telehealth has been shown to have positive health outcomes and to be associated with high rates of acceptance by patients and clinical staff in trials and real-world analysis of telehealth programs in the United States and UK. For example, in diabetes control, daily real-time monitoring of blood glucose and blood pressure resulted in better survival outcomes and glucose control. This could be expected to translate into less co-morbidity and fewer resulting hospitalisations (e.g. cardiac and ophthalmologic complications of diabetes). In patients with diabetes, chronic obstructive pulmonary disease, or heart failure, telehealth use has been shown to result in significantly fewer admissions to hospital over a 12-month period.***
Time to embrace telehealth technologies in Australia
Despite visible results in the UK and US, Australia has been relatively slow in its uptake of telehealth technologies. One ‘fear factor’ component is whether telehealth will replace face-to-face consultations – and this has been the question on everybody’s mind, especially with health providers. But it definitely will not. In fact, implementing telehealth solutions may increase face-to-face consultation at the right time as with decision support tools, the healthcare provider may see the need to have a consultation before the patient’s actual visit.
Another key barrier to adoption in Australia is that primarily from the health providers perspective, the platforms operate in silos. There is no unified or single source of information or interoperability among the platforms making it very hard for clinicians to use.
For instance the video consultation is on a separate platform to where the patient record is stored. During the consultation, the clinician has to juggle between two software platforms making it time consuming.
Another real-time example is with the clinical data. Clinicians do not want the whole gamma of raw clinical data like blood pressure, blood glucose from the personal health devices, instead want an analysed data which can help them their decision for managing patient condition.
But if we can have a centralised software platform that can provide the 3 components of tele-Health and integrating with centralised patient record system – My Health Record, it would dramatically increase the uptake of such services by the clinicians.
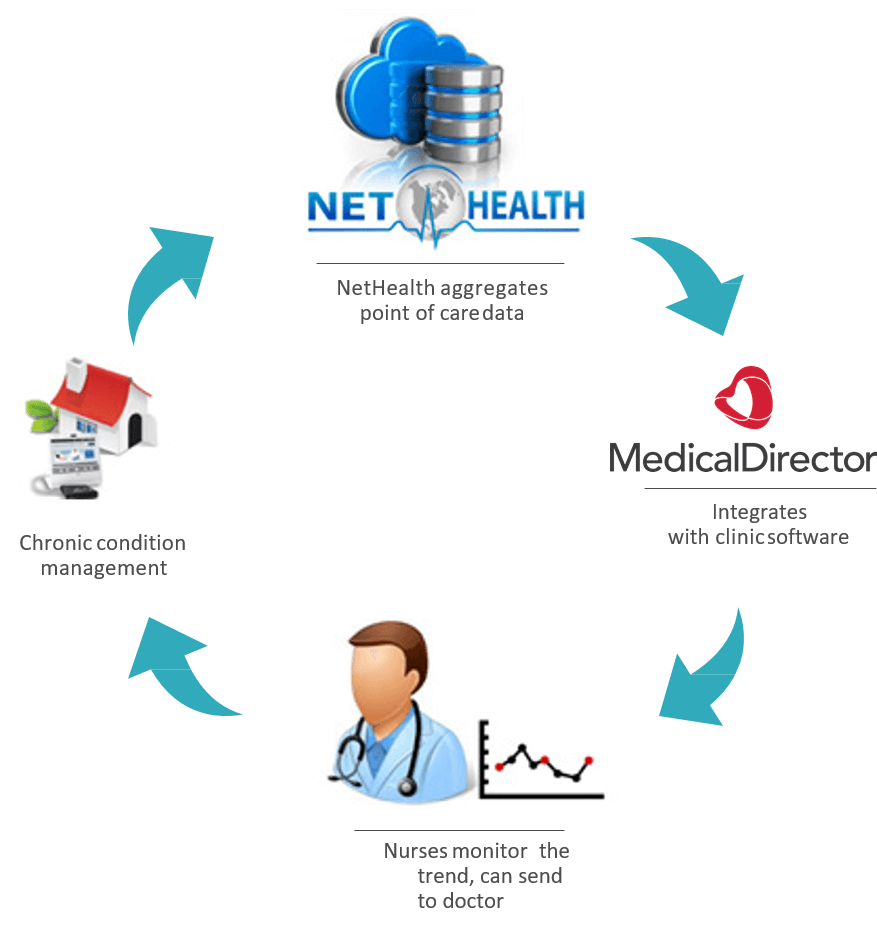
Net-HealthData is one such software platform that has the decision support tool and the active coaching and monitoring components of telehealth, while working on the third element of video consultation as well. With the healthcare team like diabetes educators, dieticians, psychologists, exercise physiologists available in-house, the patients are monitored for their clinical data, coached and motivated to keep them healthy. The analysed data is sent to the patients’ clinician regularly, which provides the continuity of patient care. By integrating with major clinic management software MedicalDirector, the platform is easier to use and has a centralised patient record system.
For more information about Net-HealthData visit http://www.net-health.com.au
References
* The Royal Australian College of General Practitioners. Vision for general practice and a sustainable healthcare system. Melbourne: RACGP; 2015
** R. Sparks, B. Celler, C. Okugami, R. Jayasena and M. Varnfield, “Telehealth Monitoring of Patients in the Community,” Journal of Intelligent Systems, vol. 25(1), pp. 37-53, 2016.
***A. Steventon, M. Bardsley, J. Billings, J. Dixon, H. Doll, S. Hirani, M. Cartwright, L. Rixon, M. Knapp, C. Henderson, A. Rogers, R. Fitzpatrick, J. Hendy and S. Newman, “Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial,” BMJ, p. 344, 2012.









